Filling out the Texas Do Not Resuscitate (DNR) Order form is a critical step for those who wish to ensure that their wishes regarding resuscitation are known and honored by healthcare professionals. However, errors can occur during this process, which can lead to unwanted consequences. Here are ten common mistakes made when completing this form.
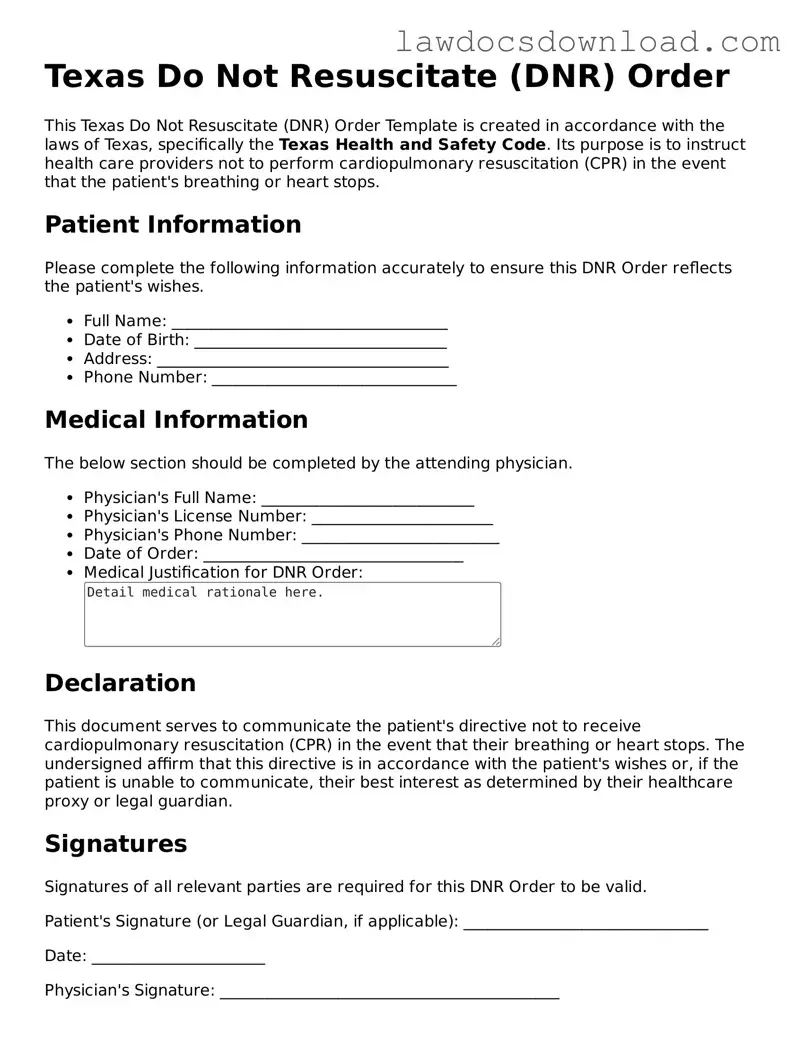
One of the most frequent mistakes is not properly verifying the identity of the individual the DNR applies to. This mistake can lead to confusion and delays in emergency situations. It is essential that every detail, including full name and date of birth, matches the individual's legal documents.
Another common error is the lack of a valid signature. For a Texas DNR Order to be legal, it must be signed by the person to whom it applies, or in certain cases, by their legally authorized representative. Without this signature, the document may be considered invalid.
Incorrectly dating the document or failing to date it at all is also a common oversight. The date the DNR Order is signed is critical as it indicates when the order became effective. Missing or incorrect dates can cast doubt on the validity of the document.
Many people fail to discuss their DNR Order with their family or healthcare proxy. This oversight can lead to surprise or disagreement among family members or healthcare professionals in an emergency, causing unnecessary stress and potentially undermining the individual's wishes.
There is also the mistake of not including a physician’s signature. In Texas, a DNR Order must be signed by a physician to verify that the individual has been informed of the implications and that the order reflects the person's current wishes regarding resuscitation.
Some individuals neglect to make enough copies of their DNR Order. It is advisable to have copies readily available to provide to healthcare providers, to keep at home, and to share with a healthcare proxy or family members.
Omitting relevant health information is another error. The DNR form should include any pertinent medical information that healthcare professionals need to know, which can affect the care provided in an emergency situation.
Keeping the DNR Order in an inaccessible place can also negate its effectiveness. It's important that the document is easily accessible in an emergency. Informing family members and healthcare providers of its location is equally important.
Not reviewing and updating the DNR Order regularly can lead to issues as well. As health conditions change, the DNR Order may need adjustment. It is recommended that the document be reviewed periodically and after any major health decisions.
Lastly, a common mistake is not consulting with a healthcare professional when completing the DNR Order. This can result in misunderstandings about the implications of the order. Guidance from a healthcare professional can help ensure that the document accurately reflects the individual’s wishes.
By avoiding these mistakes, individuals can ensure that their Texas DNR Order is properly executed and effective, providing peace of mind that their wishes regarding resuscitation will be respected.