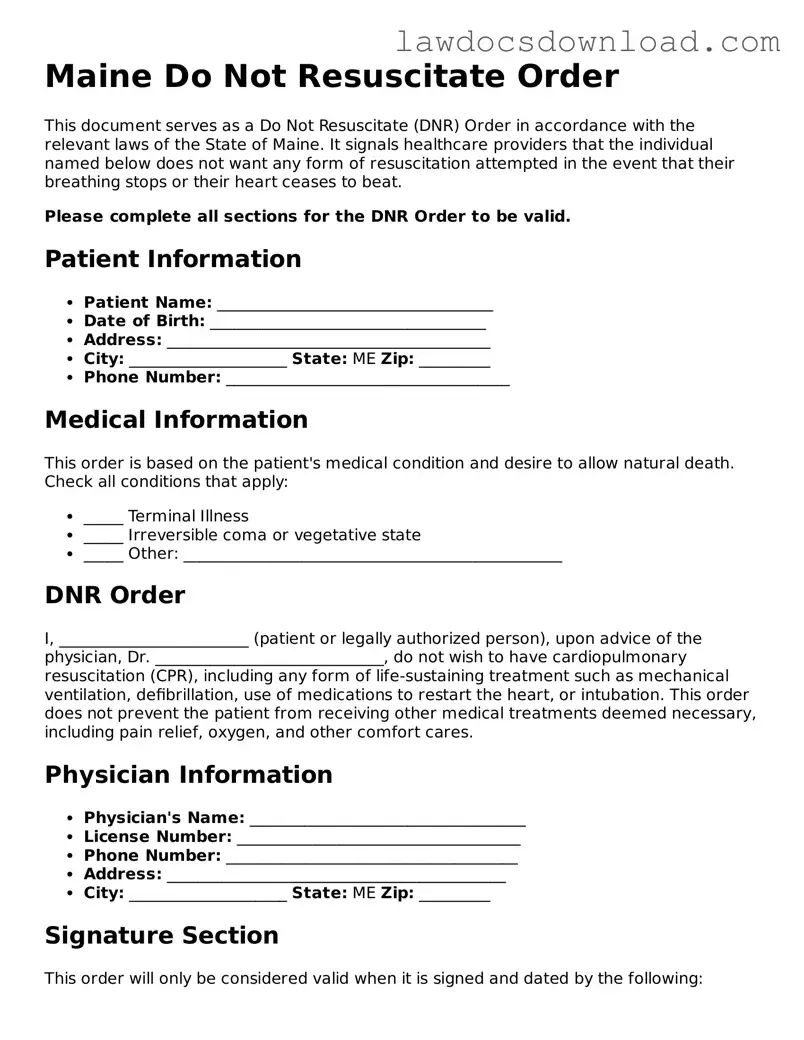
Legal Maine Do Not Resuscitate Order Form
A Maine Do Not Resuscitate Order form is a legal document that communicates a person’s wish to not receive cardiopulmonary resuscitation (CPR) in the event their heart stops or they stop breathing. This form is used by those who want to ensure that their healthcare preferences are respected during emergency situations. It’s crucial for people with terminal illnesses or those in advanced stages of chronic diseases who prefer to decline life-extending procedures.
Launch Do Not Resuscitate Order Editor Here
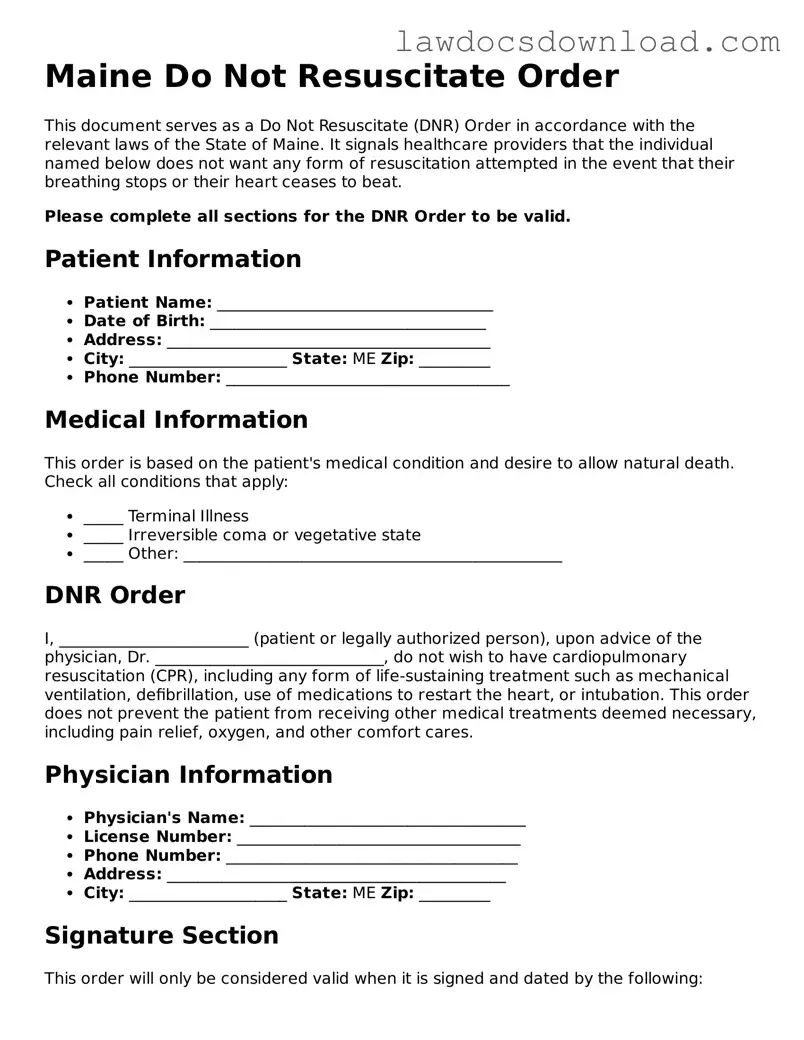
Legal Maine Do Not Resuscitate Order Form
Launch Do Not Resuscitate Order Editor Here
Launch Do Not Resuscitate Order Editor Here
or
Free Do Not Resuscitate Order
Get this form done in minutes
Complete your Do Not Resuscitate Order online and download the final PDF.