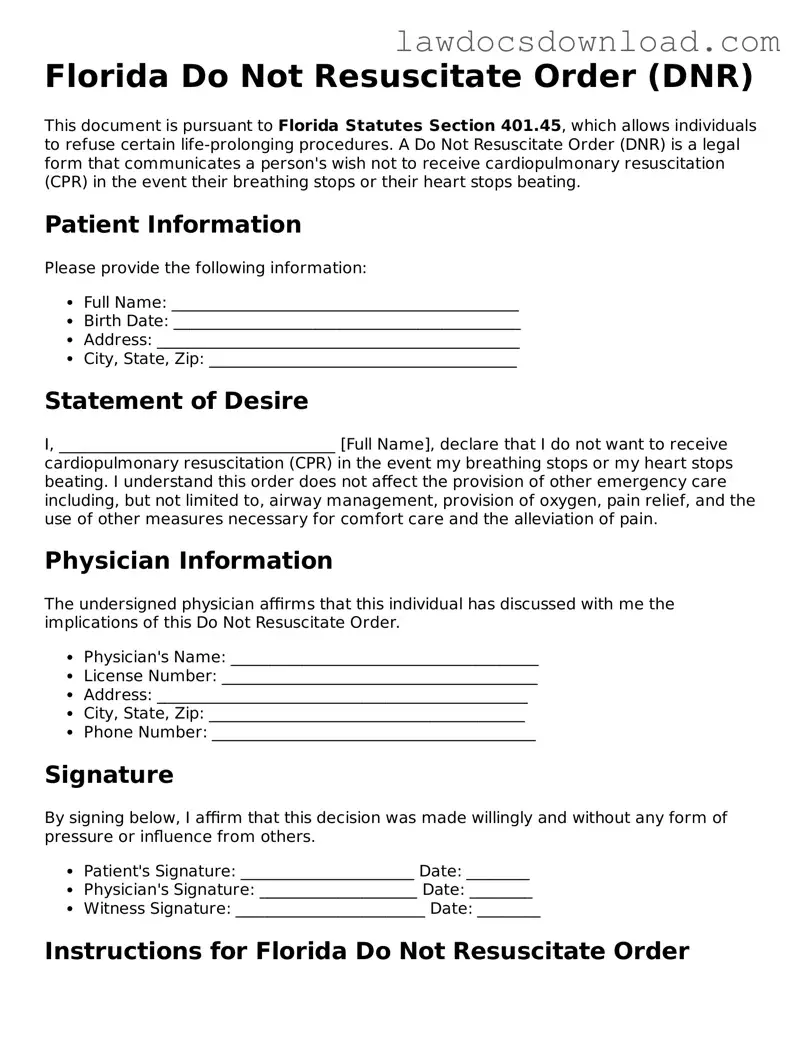
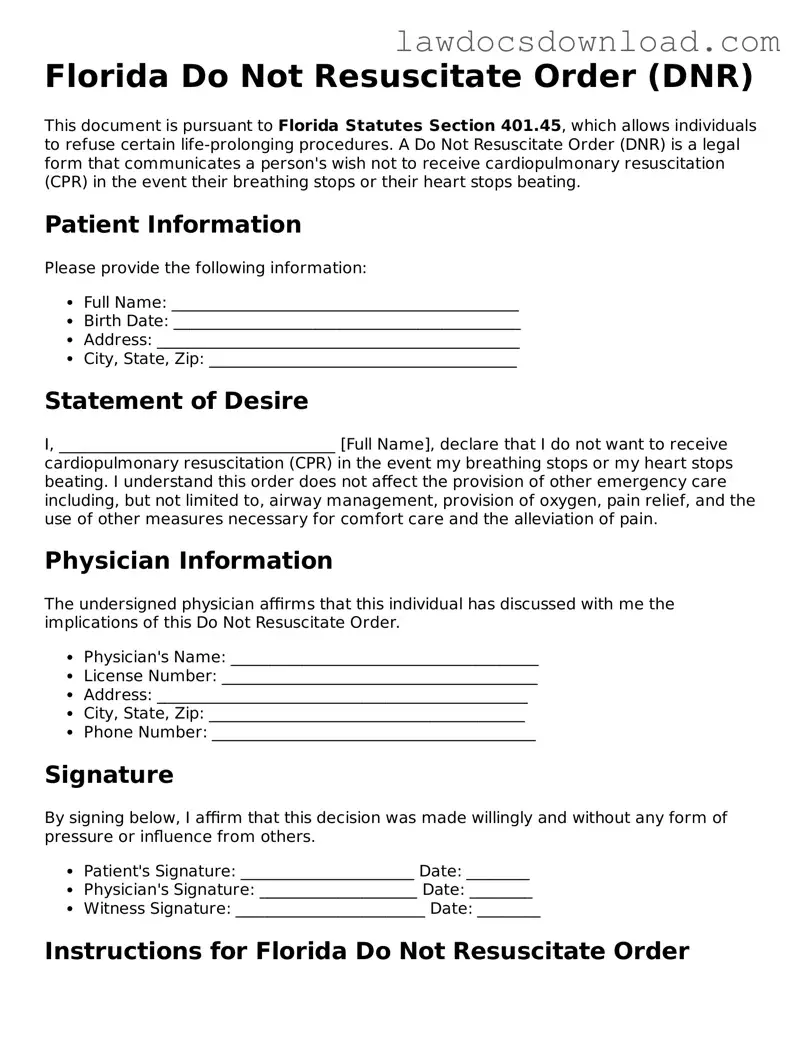
Filling out the Florida Do Not Resuscitate Order (DNRO) form is a critical step for those wishing to express their desires regarding life-sustaining treatment. However, individuals often make mistakes during this delicate process. One common error is the failure to ensure that the person signing the form has the legal authority to do so. Only the patient, a healthcare proxy, or a legally appointed guardian can validly sign the DNRO, making it crucial to verify the signatory's authority.
Another frequent misstep involves not using the most current form version. The State of Florida occasionally updates the DNRO form to incorporate changes in healthcare law or policy. Utilizing an outdated form can lead to the DNRO being considered invalid, which might result in unwanted medical interventions.
Incorrectly filling out the patient's information is also a prevalent mistake. The DNRO form requires accurate details about the patient, including their full name and date of birth. Any discrepancies between the information on the form and the patient's legal identification can render the document ineffective at a critical moment.
It's also common to overlook the necessity of a witness's signature. The presence of a witness who can attest to the authenticity of the signature adds a layer of verification to the process. Without this, the DNRO's legality can be questioned by healthcare providers.
Some individuals mistakenly believe that a lawyer's review or notarization is required for the DNRO to be valid. However, in Florida, this is not the case, and misunderstanding this can lead to unnecessary delays and expenses. The form is designed to be straightforward and does not need legal or notarial endorsement to be effective.
Not discussing the DNRO with the patient's healthcare team is another common oversight. Communication with healthcare providers ensures that the DNRO is integrated into the patient's medical records and that the medical team is aware of the patient's wishes, promoting a unified approach to the patient's end-of-life care.
Equally problematic is the belief that once completed, the DNRO does not need to be revisited. However, patients or their legal representatives should regularly review the DNRO, especially if there is a significant change in health status, to ensure that it still reflects the patient's desires.
Failure to properly distribute copies of the filled-out DNRO can lead to its instructions being overlooked when they are most needed. It's crucial to provide copies to all involved parties, including family members, healthcare proxies, and primary care doctors, to ensure that the patient's wishes are honored.
There also exists confusion about the difference between a DNRO and other advance directives, such as a living will. Each document serves different purposes and complements the other; understanding their roles can prevent critical misunderstandings regarding patient care preferences.
Lastly, a significant mistake is not safely storing the DNRO. The document should be easily accessible in an emergency. Patients or their representatives should consider keeping a copy in an easily identifiable location and informing close family members or caregivers of its whereabouts to prevent any delay in its application.