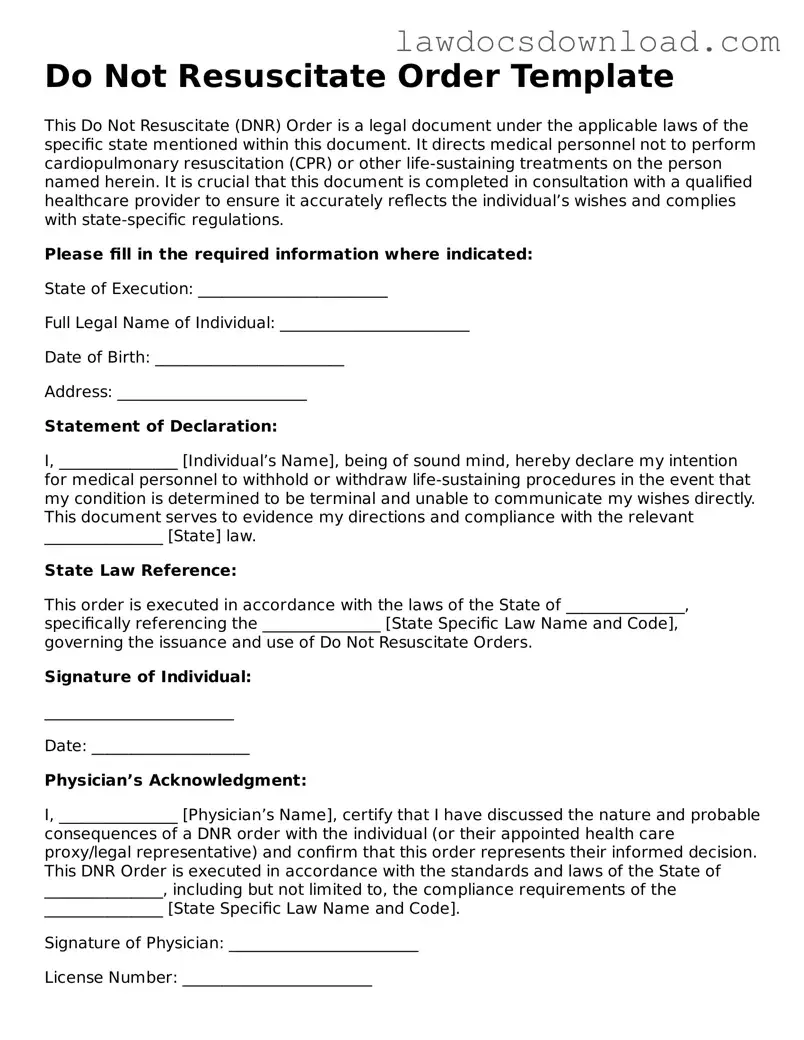
Blank Do Not Resuscitate Order Template
A Do Not Resuscitate Order form, often abbreviated as DNR, is a legal document that prevents medical professionals from performing CPR (cardiopulmonary resuscitation) if a patient's breathing stops or if the heart stops beating. It is specifically designed for individuals with serious illnesses or those at the end of life who choose not to undergo certain life-saving measures. The form must be completed and signed by both the patient and their healthcare provider to be valid.
Launch Do Not Resuscitate Order Editor Here
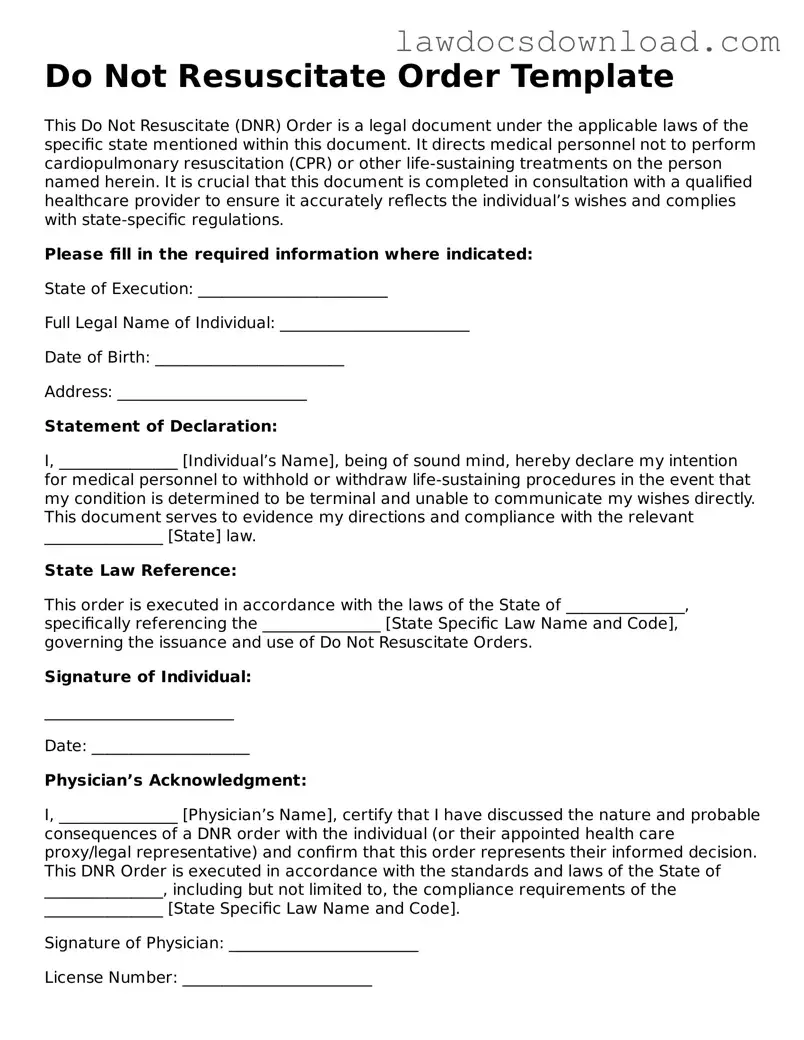
Blank Do Not Resuscitate Order Template
Launch Do Not Resuscitate Order Editor Here
Launch Do Not Resuscitate Order Editor Here
or
Free Do Not Resuscitate Order
Get this form done in minutes
Complete your Do Not Resuscitate Order online and download the final PDF.